Gut health has emerged as a significant focus in wellness and medicine due to ongoing research in recent decades. Once considered just a simple digestive system responsible for breaking down food and absorbing nutrients, the gut is now believed to play a far more critical role in our overall health. Not only is a healthy gut crucial for digestive efficiency, but it’s also intimately connected to various aspects of systemic health, including but not limited to immune function, mental health, and chronic disease management. In this blog we will review what gut health means, factors that contribute to poor gut health, and the far-reaching impact it has on systemic well-being.
What is Gut Health?
The term of “gut health” represents the health of the entire digestive tract, which includes the esophagus, stomach, small intestine, and large intestine. This intricate system serves as the habitat for a diverse microbial ecosystem, comprising trillions of bacteria, viruses, and fungi, collectively referred to as the gut microbiota. Balance within this microbial community is integral for a multitude of physiological functions, including optimal digestion, efficient nutrient absorption, vitamin production and robust immune responses.
Gut health can be gauged through a variety of indicators, each providing insights into the functional status of the digestive system:
Digestive Efficiency: This refers to how effectively the digestive system absorbs and metabolizes ingested food into bio-available energy.
Microbial Balance: This pertains to the maintenance of a favorable ratio between beneficial and harmful bacterial species residing in the gastrointestinal tract. Dysbiosis refers to imbalance in this ratio.
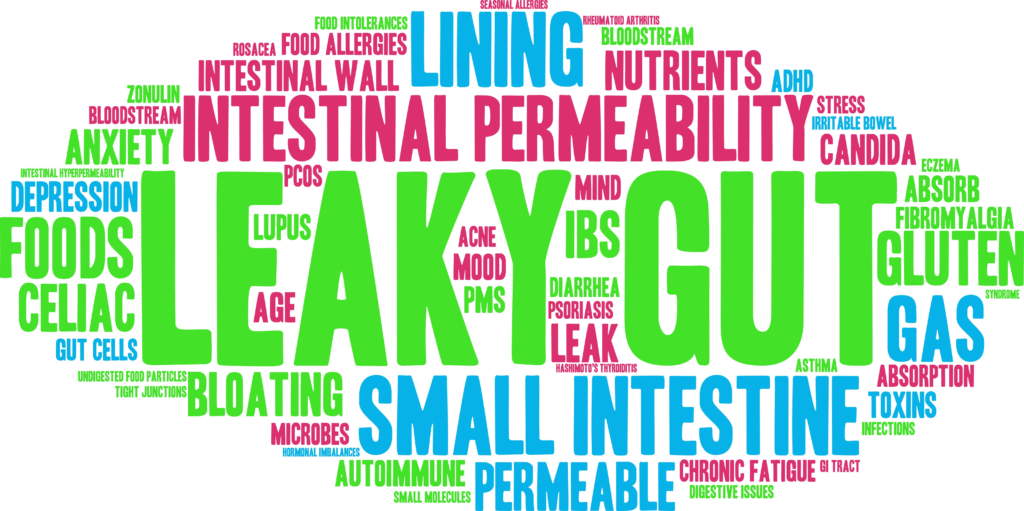
Intestinal Permeability: Known as ‘Leaky Gut’, this refers to the selective process the intestines use to regulate the transport of substances across the intestinal barrier. This ensures essential nutrients are absorbed into the body while preventing harmful substances from entering the bloodstream.
Immune System Health: A well-functioning gut supports an immune system that is both responsive and discriminating, capable of mounting appropriate defenses without eliciting unwarranted inflammatory reactions.
Absence of GI Disease or Issues: An optimally functioning gut typically means an absence of any gastrointestinal (GI) conditions such as IBS, IBD, Celiac, SIBO, Diverticular disease, and common GI disturbances, such as constipation, diarrhea, and bloating.
By these measures, gut health not only influences digestive wellness but also has far-reaching implications for systemic health and overall well-being.
Are You Sabotaging Your Gut Health?

Our lifestyle plays a significant role in health of our gut:
Poor Diet: A diet rich in processed foods, high sugar, and low fiber can disrupt the balance of gut bacteria. These unhealthy foods can lead to an overgrowth of harmful bacteria, resulting in poor gut health.
Sleep Deprivation: Lack of sleep can adversely affect the gut by disrupting the natural circadian rhythm, which, in turn, can disturb the balance of our microbiome.
Antibiotics and Medications: While antibiotics are crucial in treating bacterial infections, they can also deplete beneficial bacteria in the gut. Other medications, like antacids and corticosteroids, can also negatively affect gut flora. Always consult your physician for personalized guidance.
Stress: Chronic stress not only affects mental health, but also disrupts the gut microbiome. Stress hormones can cause an imbalance in gut bacteria, leading to digestive issues and weakened immunity.
Alcohol and Substance Abuse: Excessive consumption of alcohol can damage gut lining, impacting nutrient absorption and ability to maintain a balanced microbiome.
Environmental Pollutants: Pesticides, pollutants, and chemicals in our environment can also negatively impact our gut bacteria, disrupting their balance and leading to poor gut health.
Imbalanced Gut Bacteria: The imbalance of ‘good’ and ‘bad’ bacteria, known as dysbiosis, can have a direct impact on gut health, potentially leading to gastrointestinal issues like irritable bowel syndrome (IBS) and inflammatory bowel disease (IBD).
Poor Oral Health: An overgrowth of harmful bacteria in the mouth, when swallowed, can disrupt the balance of gut microbiota. Chronic oral infections can cause systemic inflammation, potentially impacting the gut lining and contributing to cardiovascular disease and diabetes. Additionally, oral health issues can influence saliva production which is essential for the initiation of digestion. In essence, maintaining good oral hygiene is pivotal for a healthy gut & health.
Additional Factors That Contribute To Poor Gut Health
Lack of Physical Activity: A sedentary lifestyle has been linked to an unhealthy gut microbiome. Regular exercise promotes a diverse gut flora, which is beneficial for overall health.
Smoking: Tobacco smoke is harmful to the gut flora and has been linked to various gastrointestinal diseases.
Age: As we age, there are natural changes in the gut biome that can lead to poor gut health. These changes may necessitate dietary or lifestyle adjustments.
Genetics: While certain individuals have a genetic predisposition that influences their gut flora composition, it’s important to note that gut health is shaped by a combination of genetics and environmental factors, not just genetics in isolation.
Excessive Consumption of Artificial Sweeteners: Some studies suggest that artificial sweeteners can negatively impact gut bacteria and may contribute to glucose intolerance.
High-Fat Diet: Excessive saturated fats can lead to imbalance in gut microbiota, promoting inflammation and metabolic disorders.
Infections: Gastrointestinal infections caused by pathogens can wreak havoc on your gut flora, often requiring a long time to restore balance.
Impact on Systemic Health
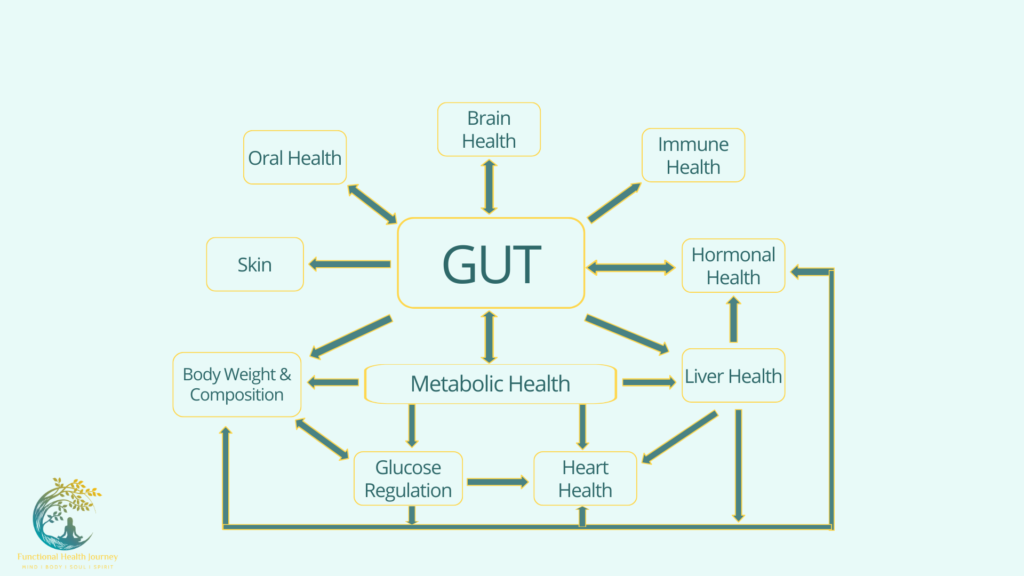
Gut microbiome research is rapidly evolving, and many aspects related to gut health and its impact on systemic health have been researched extensively in recent years & continues to evolve.
Immune Function: A healthy gut contributes to a robust immune system. 70-80% of our immune cells are located in the gut, and the gut microbiome helps in training and regulating these cells. These microbes help differentiate harmful invaders from benign entities, regulate immune responses and strengthen the gut lining, creating a barrier against harmful substances.
Therefore, a balanced gut microbiome is not only pivotal for a resilient immune system but also crucial in protecting susceptible individuals from infections, allergies, and autoimmune disorders.
Mental Health: The connection between the gut and the brain, known as the gut-brain axis, underscores how our gut health can significantly influence our mental well-being. Here are some ways they communicate:
Neurotransmitter Production: Consider our gut as a mini-factory for brain chemicals, notably serotonin. A disrupted gut can throw these chemicals off balance, affecting our mood and cognitive functions. For instance, the gut produces GABA, a calming metabolite. Along with other compounds, GABA plays a crucial role in regulating our emotions and mental state.
Inflammation: An unhealthy gut can lead to chronic inflammation, linked to mental health issues like depression and anxiety. Factors like leaky gut can intensify this inflammation. Additionally, when our immune system—which is closely tied to our gut health—becomes imbalanced, it may trigger brain inflammation, contributing to various mental health disorders.
Physical Connection & Stress Reponses: Our gut and brain have a direct line of communication through the vagus nerve. Changes in the gut can send various signals to the brain, affecting our mental state. An imbalanced gut can make our body’s stress response go haywire via the HPA axis leading to anxiety and other stress related disorders.
Helpful Compounds: Good gut bacteria create helpful compounds like GABA, B vitamins & short chain fatty acids that can have positive impact on our brain function and behavior. On the flip side, factors like a poor diet can tip this balance which then affects our mental well-being.
Blood-Brain Barrier (BBB): This barrier keeps harmful substances from reaching our brain. A disrupted gut might weaken this barrier, potentially allowing unwanted substances to pass through the BBB and influence our brain function & health
In essence, while the evidence pointing to these connections is compelling, it’s also essential to recognize the complexity of the gut-brain axis. Both are affected by a plethora of factors, and not every individual with gut disturbances will face mental health challenges. As research progresses, our understanding of this profound connection will undoubtedly deepen.
Metabolic Health:
Blood Sugar Regulation: Poor gut health has been connected with metabolic disorders like obesity and type 2 diabetes. Gut bacteria play a role in regulating blood sugar, fat storage, and even hunger hormones. This happens
Heart Health: The gut microbiome has a significant influence on heart health by affecting factors like cholesterol levels and blood pressure. Some strains of gut bacteria have been shown to break down dietary fibers into beneficial compounds called short chain fatty acids that help reduce inflammation and modulate lipid metabolism.
Liver Health: The liver is essential for detoxifying the body and is interconnected with gut health. Gut bacteria play a role in metabolizing dietary components, influencing how the liver processes various substances. Imbalances in the gut microbiome can be a contributing factor in conditions like fatty liver disease.
This connection between gut and metabolic health will be explored further in my next blog.
Hormonal Health
The gut plays an essential role in the metabolism and regulation of various hormones. Imbalances in gut health can lead to hormonal disruptions. These are just some examples.
Insulin: The gut plays a key role in regulating blood sugar. In response to food, the intestine releases hormones, such as glucagon-like peptide-1 (GLP-1), that aid in insulin production. The composition of our gut bacteria can also influence our body’s sensitivity to insulin. An imbalanced gut microbiome may shift this sensitivity, potentially heightening the risk of type 2 diabetes.
Cortisol: The relationship between cortisol and the gut is bidirectional. Chronic stress can alter the gut microbiome’s composition, reducing bacterial diversity. Conversely, a compromised gut may exacerbate the body’s stress response. Elevated cortisol over prolonged periods can lead to a host of issues that was discussed in my previous blog.
Serotonin: Approximately 90% of the body’s serotonin, a neurotransmitter that affects mood, digestion, and sleep, is produced in the gut. While this serotonin doesn’t cross into the brain, gut-derived serotonin can influence the central nervous system. Dysbiosis can disrupt serotonin production, potentially exacerbating symptoms of anxiety, depression, and other mood disorders.
Sex Hormones: The gut plays a role in managing sex hormones like estrogen. Gut bacteria can affect how estrogen is processed in the body. An imbalance in these bacteria can alter its metabolism, which might influence menstrual cycles, fertility, mood, and potentially influence the risk factors associated with hormone-sensitive conditions, including certain cancers. However, it’s crucial to note that many factors play a role in these conditions, and research is ongoing.
Additional Facets of Systemic Health
Research is probing the ties between the gut microbiome, chronic disease as well as other health conditions. While evidence is growing in certain areas, it’s important to recognize that a comprehensive understanding of the full implications requires further study in this emerging field.
- Autoimmune Conditions
- Skin Health
- Autism
- Cancer
- Inflammatory Bowel Disease
- Respiratory Health
- Bone Health
- Kidney Health
- Neurological Disorders
- Longevity and Aging
R-E-C-O-G-N-I-S-E (British spelling) Signs and Symptoms of Poor GUT Health, Dysbiosis, and Gut Inflammation
R – Reflux and Heartburn: Occurs when stomach acid or bile irritate the esophagus, causing a burning sensation in the chest (heartburn). GERD can also be linked to low stomach acid, which leads to incomplete digestion, gas production which then allows stomach contents to flow back into the esophagus.
E – Excessive Gas and Bloating: While some gas is normal, excessive post-meal bloating or gas may suggest gut bacteria/yeast imbalances or poor digestion.
C – Constipation or Diarrhea: Any significant change in bowel habits, whether it’s infrequent bowel movements or loose stools, might indicate a gut problem.
O – Odor: Foul-smelling stools can be indicative of malabsorption or an imbalance in the gut microbiota.
G – Gut Sounds: Excessive rumbling or gurgling sounds from the stomach or intestines, known as borborygmi, can indicate that food isn’t moving smoothly through the digestive system or there’s an imbalance of gut bacteria.
N – Nausea and Vomiting: Persistent nausea or vomiting episodes might indicate digestive system issues, including gut bacteria imbalances or inflammation.
I – Intolerance to Foods: Developing sensitivity or intolerance to certain foods, might suggest issues with gut health.
S – Stomach Pain or Cramps: Persistent or recurrent stomach pains can be a sign of numerous gut issues, from simple indigestion to more serious conditions like inflammatory bowel disease (IBD).
E – Energy Depletion: Poor gut health can lead to nutrient malabsorption, resulting in fatigue and lack of energy.
Additional Signs and Symptoms
Weight Changes: Unexplained weight gain or loss could be tied to gut health. This can arise due to malabsorption or changes in gut bacteria that affect how nutrients and calories are absorbed as well as how hormones are impacted.
Food Cravings: An imbalance in gut bacteria might lead to increased cravings for sugar, as some harmful bacteria thrive on sugar.
Bad Breath: Chronic bad breath, or halitosis, might be linked to imbalances in the stomach or intestines.
Skin Issues: Conditions like eczema, rosacea, or acne might be tied to poor gut health.
Autoimmune Conditions: Some studies suggest that a compromised gut can increase systemic inflammation and may trigger or worsen certain autoimmune conditions.
Frequent Infections or Illness: A weakened gut can compromise the immune system, making one more susceptible to infections.
Mental Health: Memory, difficulty concentrating, headaches, anxiety, depression can be associated with gut health.
Restoring Gut Health – Some Practical Steps You Can Take!
Diverse Diet: Include fiber-rich foods, whole grains, lean proteins, healthy fats, and fermented foods into your diet.
Probiotics and Prebiotics: Aid in restoring a healthy balance of gut bacteria.
Limit your Alcohol Intake: Excessive alcohol contributes to leaky gut & inflammation.
Stay Hydrated: Water supports mucosal lining in the intestines.
Regular Exercise: Enhances the diversity and abundance of beneficial gut bacteria.
Mindful Living: Manage stress and ensure adequate sleep to promote gut health.
Optimize Oral Health & Hygiene: Make brushing, flossing, and regular dental check-ups a priority. Your body will thank you!
Conclusion
Navigating the complex realm of gut health, it is evident that the gut isn’t just a digestive powerhouse but also vital to our overall well-being. The intricate balance of our microorganisms has far-reaching effects, influencing everything from our daily mood and energy levels to our risk of chronic diseases. It is important to note that a combination of genetics plus environmental factors are involved in disease expression.
Understanding the pivotal role that our gut plays is the first step toward safeguarding our health. In an era where our lifestyle choices, from the foods we eat to the stress we encounter, can deeply impact our gut health, it’s imperative to make informed decisions. By balancing our gut biome, we’re not only nurturing our digestive health but also fortifying our body’s defenses, optimizing mental clarity, and laying the groundwork for long-term health.
As research continues to uncover the connections between the gut and other body systems, one message is clear: taking care of our gut is synonymous with taking care of ourselves. Embracing a holistic approach that includes a balanced diet, regular exercise, stress management, and adequate sleep can set us on a path towards optimal gut health and, consequently, a healthier, more vibrant life.
**Please be aware that disease risks are complex and multifactorial. The content provided in this blog is for general informational purposes only.
For a personalized guidance and to assess your gut health, please schedule a consultation.
References & Further Reading
Please note that you will find links to abstracts only for some references below:
Fung TC. (2020). The microbiota-immune axis as a central mediator of gut-brain communication. Neurobiol Dis, 136, 104714. Epub 2019 Dec 14.
Di Tommaso N, Gasbarrini A, Ponziani FR. (2021). Intestinal Barrier in Human Health and Disease. Int J Environ Res Public Health, 18(23), 12836.
Zhang Y-J, Li S, Gan R-Y, Zhou T, Xu D-P, Li H-B. (2015). Impacts of gut bacteria on human health and diseases. Int J Mol Sci, 16(4), 7493-519.
Kelly JR, Kennedy PJ, Cryan JF, Dinan TG, Clarke G, Hyland NP. (2015). Breaking down the barriers: the gut microbiome, intestinal permeability and stress-related psychiatric disorders. Front Cell Neurosci, 9:392. eCollection 2015.
Zhu S, Jiang Y, Xu K, Cui M, Ye W, Zhao G, Jin L, Chen X. (2020). The progress of gut microbiome research related to brain disorders. J Neuroinflammation, 17(1), 25.
Fassarella M, Blaak EE, Penders J, Nauta A, Smidt H, Zoetendal EG. (2021). Gut microbiome stability and resilience: elucidating the response to perturbations in order to modulate gut health. Gut, 70(3), 595-605.
Khoshbin K, Camilleri M. (2020). Effects of dietary components on intestinal permeability in health and disease. Am J Physiol Gastrointest Liver Physiol, 319(5), G589-G608.
Carding S, Verbeke K, Vipond DT, Corfe BM, Owen LJ. (2015). Dysbiosis of the gut microbiota in disease. Microb Ecol Health Dis, 26. eCollection 2015.
Brown BI. (2017). Nutritional Management of Metabolic Endotoxemia: A Clinical Review. Altern Ther Health Med, 23(4), 42-54.
Armani RG, Ramezani A, Yasir A, Sharama S, Canziani MEF, Raj DS. (2017). Gut Microbiome in Chronic Kidney Disease. Curr Hypertens Rep, 19(4), 29.
Konturek PC, Brzozowski T, Konturek SJ. (2011). Stress and the gut: pathophysiology, clinical consequences, diagnostic approach and treatment options. J Physiol Pharmacol, 62(6), 591-9.
Wiertsema SP, van Bergenhenegouwen J, Garssen J, Knippels LMJ. (2021). The Interplay between the Gut Microbiome and the Immune System in the Context of Infectious Diseases throughout Life and the Role of Nutrition in Optimizing Treatment Strategies. Nutrients, 13(3), 886.
Round JL, Mazmanian SK. (2009). The gut microbiota shapes intestinal immune responses during health and disease. Nat Rev Immunol, 9(5), 313-23.
Badal VD, Vaccariello ED, Murray ER, Yu KE, Knight R, Jeste DV, Nguyen TT. (2020). The Gut Microbiome, Aging, and Longevity: A Systematic Review. Nutrients, 12(12), 3759.
Rajagopala SV, Vashee S, Oldfield LM, Suzuki Y, Venter JC, Telenti A, Nelson KE. (2017). The Human Microbiome and Cancer. Cancer Prev Res (Phila), 10(4), 226-234. Epub 2017 Jan 17.
Zang Y, Lai X, Li C, Ding D, Wang Y, Zhu Y. (2023). The Role of Gut Microbiota in Various Neurological and Psychiatric Disorders-An Evidence Mapping Based on Quantified Evidence. Mediators Inflamm, 2023:5127157. Epub 2023 Feb 8.
Bastiaanssen, T. F. S., Cussotto, S., Claesson, M. J., Clarke, G., Dinan, T. G., Cryan, J. F. (2020). Gutted! Unraveling the Role of the Microbiome in Major Depressive Disorder. Harv Rev Psychiatry, 28(1), 26-39.
Avalos-Fernandez M, Alin T, Métayer C, Thiébaut R, Enaud R, Delhaes L. (2022). The respiratory microbiota alpha-diversity in chronic lung diseases: first systematic review and meta-analysis. Respir Res, 23(1), 214. Epub 2022 Aug 23.
Chen Y, Xu J, Chen Y. (2021). Regulation of Neurotransmitters by the Gut Microbiota and Effects on Cognition in Neurological Disorders. Nutrients, 13(6), 2099. Epub 2021 Jun 19.
Bear TLK, Dalziel JE, Coad J, Roy NC, Butts CA, Gopal PK. (2020). The Role of the Gut Microbiota in Dietary Interventions for Depression and Anxiety. Adv Nutr, 11(4), 890-907. Epub 2020 Jul 1.
Cuevas-Sierra A, Ramos-Lopez O, Riezu-Boj JI, Milagro FI, Martinez JA. (2019). Diet, Gut Microbiota, and Obesity: Links with Host Genetics and Epigenetics and Potential Applications. Adv Nutr, 10(suppl_1), S17-S30. Epub 2019 Jan 1.
Wiertsema SP, van Bergenhenegouwen J, Garssen J, Knippels LMJ. (2021). The Interplay between the Gut Microbiome and the Immune System in the Context of Infectious Diseases throughout Life and the Role of Nutrition in Optimizing Treatment Strategies. Nutrients, 13(3), 886.
Mills S, Stanton C, et al. (2019). Precision Nutrition and the Microbiome, Part I: Current State of the Science. Nutrients, 11(4), 923.
Rinninella E, Cintoni M, Raoul P, Lopetuso LR, Scaldaferri F, Pulcini G, Miggiano GAD, Gasbarrini A, Mele MC. (2019). Food Components and Dietary Habits: Keys for a Healthy Gut Microbiota Composition. Nutrients, 11(10), 2393.
Pietiäinen M, Liljestrand JM, Kopra E, Pussinen PJ. (2018). Mediators between oral dysbiosis and cardiovascular diseases. Eur J Oral Sci, 126 Suppl 1, 26-36.
Joshipura K, Ritchie C, Douglass C. (2000). Strength of evidence linking oral conditions and systemic disease. Compend Contin Educ Dent Suppl, (30), 12-23.
Chen I. (2000). The Surgeon General’s report on oral health: implications for research and education. N Y State Dent J, 66(9), 38-42.
E Lipski. (2019). Digestive Wellness: Strengthen the Immune System and Prevent Disease Through Healthy Digestion. 5th ed.
Zhao Y, Wang Z. (2020). Gut microbiome and cardiovascular disease. Curr Opin Cardiol, 35(3), 207-218.
Zhu Y, Shui X, Liang Z, et al. (2020). Gut microbiota metabolites as integral mediators in cardiovascular diseases (Review). Int J Mol Med, 46(3), 936-948.
Hansen TH, Gøbel RJ, Hansen T, et al. (2015). The gut microbiome in cardio-metabolic health. Genome Med, 7(1), 33.

